Written by Hamad Zafar, DPM, PGY-2 at Kaiser Permanente Santa Clara Podiatric Surgery Residency Program while on Global Health rotation…
Da Nang General Hospital and Da Nang Orthopedic and Rehabiliation Hospital – Da Nang Vietnam – Stutee Khandelwal, MD
Posted by Stutee Khandelwal, MD (a third year Internal Medicine/MPH resident from Kaiser Permanente, Oakland while on a global health elective in Da Nang, Vietnam at Da Nang General Hospital and Da Nang Orthopedic and Rehabilitation Hospital).
I was the second KP internal medicine resident to go to DaNang General Hospital in Vietnam (see Dhruv Verma’s blog as well). The rotation was initially set up for the orthopedic and rehabilitation hospital, but is now being expanded to include the Da Nang General hospital.
June 27-July 2: Rehabilitation, Podiatry
My start at Da Nang General Hospital was delayed due to paperwork so I accompanied my KP attending (a podiatrist) at the rehabilitation hospital for the first week. There I saw a variety of cases such as strokes (hemorrhagic> ischemic), Sudeck’s dystrophy, unrepaired congenital valvular defects leading to strokes, Beri-Beri leading to peripheral neuropathy in an alcoholic and so on. I exchanged ideas on diagnosis and management with the PMNR physicians. However most times they did not have medical records of the patient and did not know details of the previous hospitalization leading up to rehabilitation. One of the days, I led a rapid response on a patient with hypertensive urgency without any continuous cardiac or pulse ox monitoring and where the patient’s family member had to run and get nitroglycerin from the pharmacy outside!
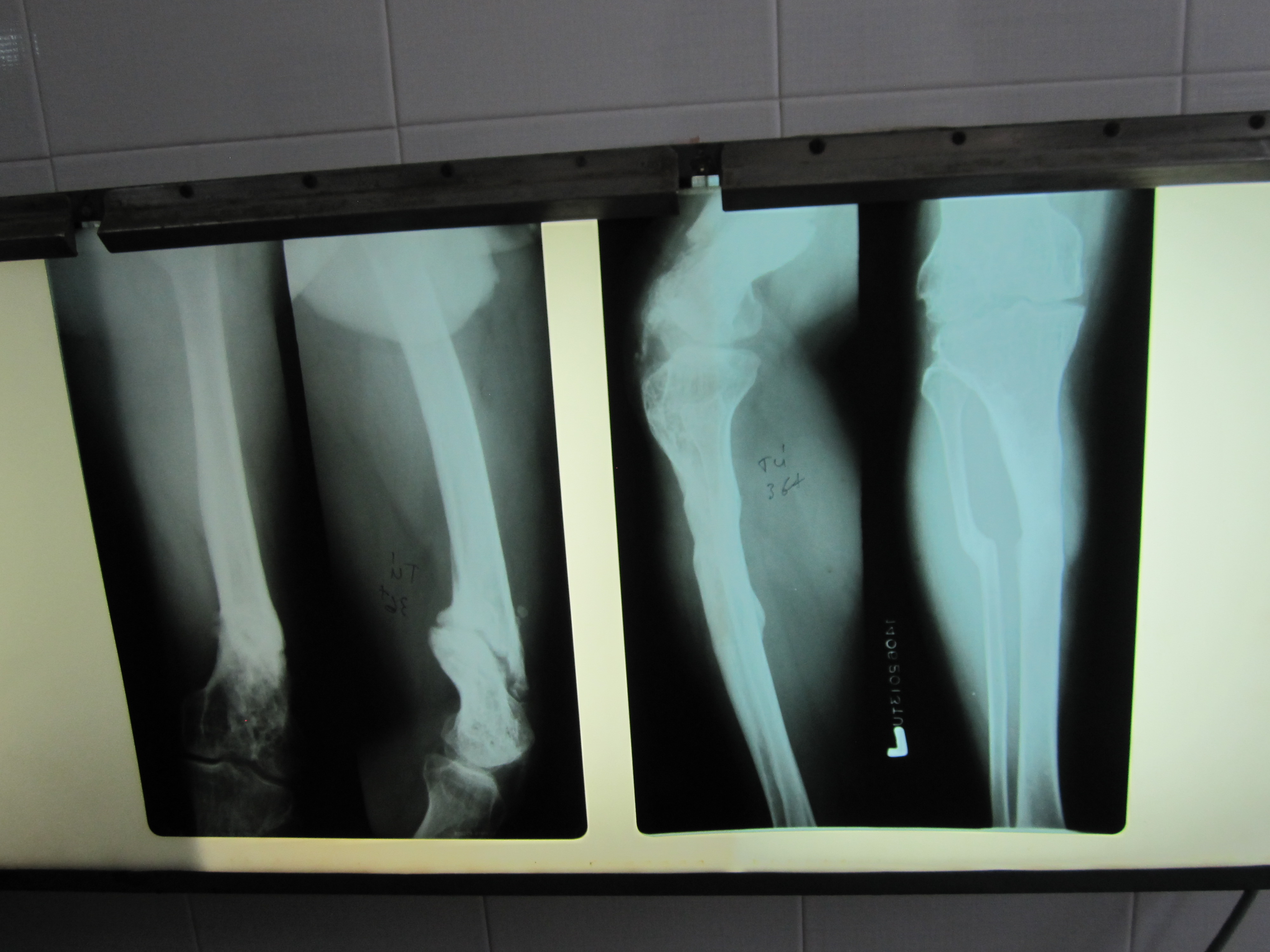
One day I accompanied the podiatry team and we saw close to 50 cases in 8 hours in the outpatient clinic. The pathology ranged from congenital defects such as fibular hemimelia to war injuries with residual shrapnel in soft tissue, to motorbike and work accidents. We saw lots of cerebral palsy, few chronic osteomyelitis (decades of drainage and pain), poorly healed fractures, a case of TB in the foot and possible case of polio (we speculated based on history that the patient possibly had an attack of acute polio leaving her with residual weakness and paralysis). I provided the pre op evaluation where the H&P sometimes changed the management for example, a case of an elderly man with chronic osteomyelitis whose limb could be salvaged as long he had a good post op follow up and home wound care, however I found out that he lived 150Km away, so we decided on a BKA instead. I would provide alternate diagnosis for a foot drop such as neuropathy based on my exam, request blood work and MRIs, and ultrasounds. It turned out to be a multidisciplinary approach as there were physical therapists from the US as well.
The next couple of days I scrubbed into the OR and observed the podiatrists work with minimal tools and anesthesia support. I performed a soft tissue mass excision from the foot under the supervision of my attending and was very impressed with the surgical assistants in the OR. The physicians spoke some broken English but the Google translator app on my phone came in very handy.
July 3- July 6: ED
The ED was a very high volume (up to 250 patients a day), efficiently run department where all the staff operates in one hall, all the patients are on gurneys side by side and physicians see them in less than 5 minutes, order labs and imaging and based on the results quickly transfer them to specialty departments. Registration, insurance and billing, nursing orders, physician note writing- all happens right then and there behind a long desk. I saw an immense variety of cases- trauma, various crush injuries, GI and pulmonary infections, pneumothoraces, SVT (use of ocular massage), poisoning (use of gastric lavage), panic attacks, and major depression and so on. There was only one “red room” with limited resources, for example, antibiotics were not given, nitroglycerin was not given for chest pain, intubation was deferred to the ICU unless absolutely necessary. The ED physicians worked in teams and took turns to do overnight call. Evening and nights were the highest volume due to lots of motorbike accidents especially combined with intoxication. I was very impressed with the promptness of consultants coming down to the ED and making their recommendations. All the on call physicians stayed in the hospital and since there weren’t any residents, I got to interact with the senior physicians and chiefs of the departments, who were all quite approachable and friendly. While I was there, a group of French students were also shadowing and I took the opportunity to do some bedside teaching with them.
July 7-11: Cardiology
Cardiology was the largest inpatient department in the hospital. Any patient with a cardiac history (active or not) was sent to cardiology, be it for a UTI or for a pneumonia. The cardiology chief was very welcoming and did some one on one bedside teaching with me. I followed a few patients during my time there- endocarditis with Janeway lesions and splinter hemorrhages, post partum cardiomyopathy, stroke, and acute fulminant liver failure. I vividly remember the extensive use of acupuncture inpatient for stroke rehabilitation. Another highlight of my inpatient experience was watching how efficiently all the appropriate disciplines worked together to discuss a case of renal failure in a patient with endocarditis, where an infarct was seen on CT. The cardiology chief arranged for a meeting the next day and all the heads of the departments- ID, Renal, Radiology, Pharmacy, General Surgery and Vascular surgery came together and took turns to give their opinions and came to a consensus on the management in less than an hour. I also toured the cath lab, echocardiography, pediatric CT surgery departments. One day after work, I shadowed the cardiology chief in his private clinic where he see saw the whole spectrum of internal medicine ranging from ultrasound diagnosis of worm infestation in the GI tract to cervical arthritis. He even took X-rays on his own, had a small laboratory and IV set up in the back!
July 12: Infectious Disease and field trip
On one of the free days, I visited the ID department where I saw several cases of dengue, rare cases of chronic TB meningitis and crytococcal meningitis. In the afternoon, the French students and I took a tour of the neighboring hospitals- women and children, cancer hospital, and I also visited the lab services at DaNang General. I was impressed with the technology, the work ethic of the staff, the cordial and courteous nature of the people in general.
July 13- July 16: ICU
The ICU was a busy place with at least 20-40 active patients at a time, aside from several chronic ventilator patients such as those with Lou Gehrig’s disease, and another 20-30 “TCU” level patients. The pathology was fascinating- various manifestations of TB, poisonings (rat poison, snake venom, insecticide, neurotoxins) as suicide attempts among men and women from the rural areas, burkholderia pneumonia in a farmer, VRE urosepsis, and one fascinating case of locked in syndrome due to a snake bite. The physicians worked on a 3 day overnight call schedule. There wasn’t a hierarchy, every one there is a “doctor” whether a fresh graduate of medical school or a seasoned physician with decades of experience. The ICU chief was a very dynamic and smart physician with training from the US, so I would often discuss cases with him. He led teaching rounds if there was time, I was asked to present articles or short reviews of topics. I accompanied the physicians on consults to other departments, looked up articles, and found out that UpToDate was a quite precious and highly regarded commodity over there. I also attempted a lumbar puncture and watched a central line being placed with judicious use of basic equipment and minimal waste being generated.
An unforgettable experience was witnessing code blue in the ID department on a 92yr old man with meningitis. Shockingly, not all departments have a crash cart, so we were limited in what we could do and the patient did not survive. Code status wasn’t really discussed on admission or even during the ICU stay until the physicians inform the family members of a dire prognosis. In most cases, the family understood and waited till an auspicious day to take the patient home.
Travel: On Sundays, I took short trips to nearby tourist spots such as Lady Buddha, Marble mountain, MySon Holyland, Hue City, Hoi An and an overnight trip to Ha Long Bay on my way back to the US. These sites were beautiful, each with its unique architecture and history, and some with breathtaking landscape like Ha Long Bay. I met other travelers and travelled in groups by taxi.
Climate: It was very hot all day and night, usually around 90-100 degrees. Sun screen, cotton and linen clothing came in handy and I kept myself well hydrated.
Food: Challenging since I was vegetarian, but if you like seafood and meat, tons of great and cheap options. Luckily I never fell sick even with roadside foods (thanks to growing up in India!). The physicians I met were very kind and took me for coffee/dessert after work or even invited me to their homes.
Stay: I stayed in a hotel near the beach (about 6 Km away from the hospital). While it was a nice and relaxing, I would recommend staying closer to the hospital, so that you can do late or overnight night shifts. Hotels in the city tend to cheaper too. Also, there are lot of restaurants, shops, and things to do in the city.
I will always remember this wonderful and unique experience in Vietnam and highly recommend it to any resident interested in a global health elective.




Awesome blog! Is your theme custom made or did you download it
from somewhere? A design like yours with a few simple
adjustements would really make my blog shine.
Please let me know where you got your design. Thanks